A revolutionary treatment in mental healthcare, Deep TMS™ has uniquely positioned itself in the treatment landscape with FDA-clearance allowing for the treatment of late-life depression. Utilizing BrainsWay’s patented H-Coil technology, Deep TMS offers a distinctive approach by generating a magnetic field capable of penetrating deeper and broader brain regions. This ability to reach and stimulate critical brain structures can address some of the unique challenges faced by elderly patients suffering from Major Depressive Disorder (MDD).
BrainsWay’s H-Coil design can be particularly beneficial for elderly patients, where age-related increases in scalp-cortical distance can benefit from the deeper electric field generated by BrainsWay’s technology.
Repeated peer-reviewed studies have validated the efficacy of Deep TMS treatment for elderly patients. The potential to significantly improve mental health outcomes can lead to remarkable enhancement in the quality of life for those battling depression.
As a noninvasive procedure, Deep TMS is well-tolerated, has a favorable safety profile, and does not produce systemic side effects. Its convenient 20-minute sessions do not involve any significant recovery period, generally allowing for seamless integration into patients’ daily routines

Late-life depression, particularly Major Depressive Disorder (MDD), is a significant and growing concern as the global elderly population expands. MDD in the elderly often goes underdiagnosed due to overlapping symptoms with dementia, such as poor attention and concentration, complicating the diagnostic process and treatment. This demographic shift, with the elderly population expected to double to approximately 2 billion globally by 2050, underscores the urgent need for effective, tailored treatment strategies.
Studies indicate that up to 15% of community-dwelling elderly individuals experience depressive symptoms, with even higher rates in residential care settings. The prevalence of MDD in the elderly ranges from 1% to 5% in the community and rises to 13.5% among those requiring home healthcare. This high prevalence highlights the necessity for heightened awareness, improved diagnostic accuracy, and better therapeutic approaches to manage depression in this vulnerable and growing segment of the population.
Many treatment options exist for managing late-life depression, each with unique benefits and limitations. Deep TMS, in particular, has demonstrated safety and efficacy in clinical studies, successfully addressing many of the challenges in treating elderly patients.

Medication:
Antidepressants, including selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), and tricyclic antidepressants (TCAs), are commonly prescribed to treat late-life depression. These medications work by altering the balance of neurotransmitters in the brain, such as serotonin, norepinephrine, and dopamine, which are associated with mood regulation. SSRIs and SNRIs are often preferred due to their favorable side effect profiles compared to TCAs. Evidence supports their efficacy in reducing depressive symptoms in older adults, but non-response rates can be as high as 55%, highlighting the need for alternative therapies. Elderly patients often face higher non-response rates, risk of adverse drug-drug interactions due to polypharmacy, and susceptibility to side effects like hyponatremia and increased fall risk.
Psychotherapy:
Cognitive-Behavioral Therapy (CBT) is a structured, time-limited therapy focusing on identifying and changing negative thought patterns and behaviors associated with depression. It involves developing coping strategies, problem-solving skills, and positive behaviors with a therapist. Studies have demonstrated that CBT can be as effective as medication for some patients, particularly in mild to moderate cases, and it avoids pharmacological side effects. However, accessibility to trained therapists and physical or mobility limitations can make it difficult for elderly patients to attend regular sessions, and cognitive impairments can hinder engagement.

Neurostimulation Modalities:
Electroconvulsive Therapy (ECT) involves administering electrical impulses to the brain under general anesthesia to induce controlled seizures, which can quickly reduce severe depressive symptoms. Meta-analyses confirm its efficacy, particularly in treatment-resistant cases. However, ECT’s side effects, such as memory loss and confusion, are significant, especially in older adults, and the procedure’s need for anesthesia and hospital visits can be taxing.
Repetitive Transcranial Magnetic Stimulation (rTMS) is a non-invasive procedure using magnetic fields to stimulate specific brain areas involved in mood regulation. Administered daily over several weeks, clinical trials have shown its effectiveness in treating depression. However, the outcomes achieved with older age patients have been limited relative to those achieved with younger patients treated with rTMS, likely due to age-related brain atrophy and other factors.
Deep Transcranial Magnetic Stimulation (Deep TMS) uses specialized H-coils to reach deeper and broader brain areas compared to traditional rTMS, aiming to overcome some of these limitations. Recent studies show promise for Deep TMS in treating late-life depression, as demonstrated below.

Other Evidence-Based Treatments:
Regular physical activity, such as walking, swimming, or yoga, can improve mood and overall well-being by releasing endorphins and promoting better sleep. Even moderate exercise can significantly benefit mental health, but mobility issues and chronic health conditions can make it difficult for some elderly individuals to engage regularly.
Social support and engagement through group activities, volunteering, or maintaining regular contact with family and friends can significantly reduce loneliness and depression. Research indicates that social support can improve treatment outcomes, but social isolation due to loss of loved ones or physical limitations can hinder engagement.
Proper nutrition supports overall health, including mental well-being. Diets rich in omega-3 fatty acids, vitamins, and minerals are linked to lower depression rates, with specific interventions like the Mediterranean diet showing promise. However, dietary restrictions and conditions affecting nutrient absorption complicate nutritional interventions.
Open-label, naturalistic data assessed Deep TMS’s safety and efficacy in late-life depression in 247 patients aged 60-91 receiving 20 or more sessions. These patients had an average history of 8.5 depressive episodes and were on average taking 12 concomitant antidepressant medications.
Results showed that after 30 sessions, there was a response rate of 79.4% and a remission rate of 60.3% on the most-rated scale. The median onset of response was 14 sessions (20 days), and for remission, it was 15 sessions (23 days).
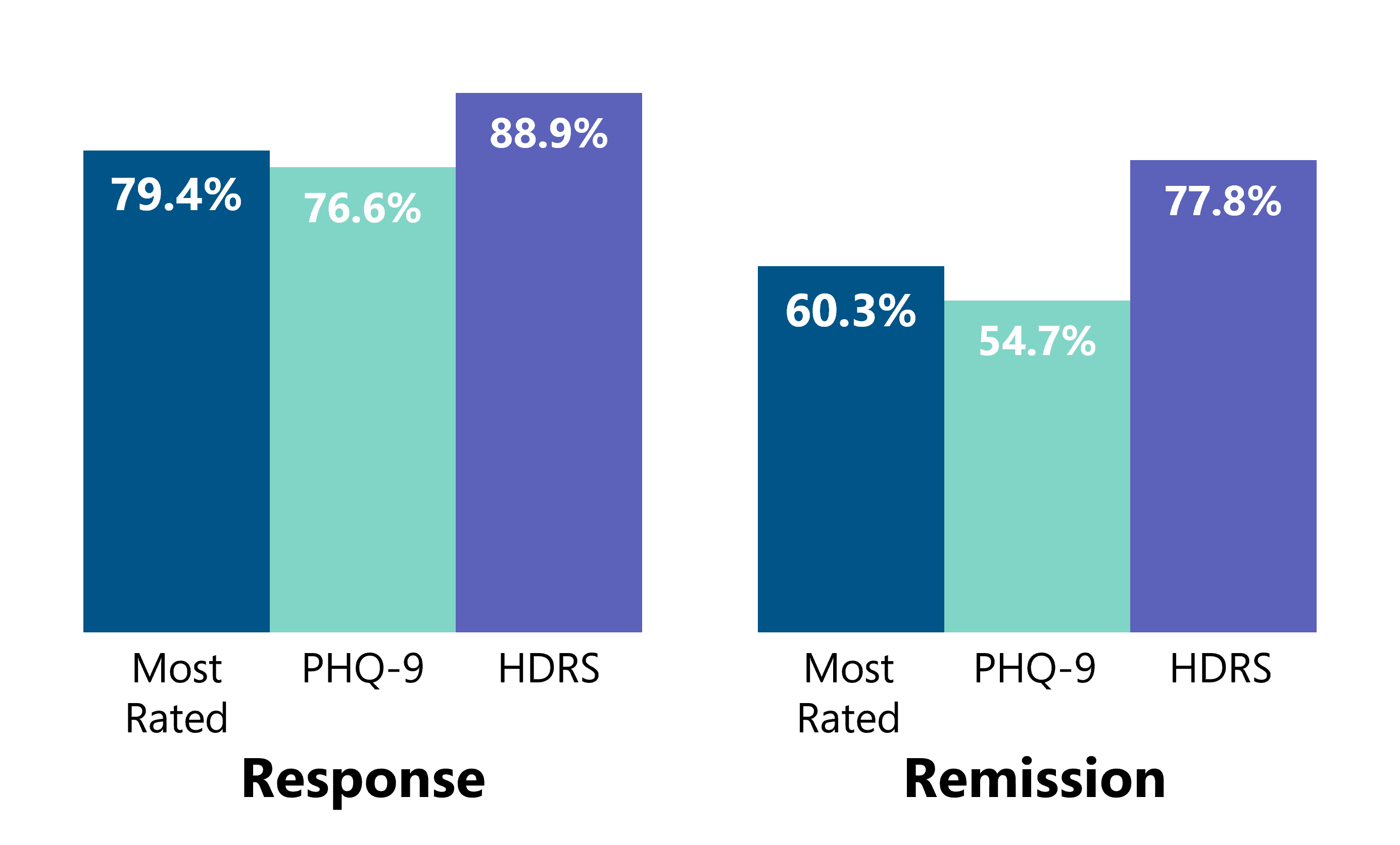
Comparing these results with a recent large naturalistic study of Deep TMS in middle-aged adults with MDD, the response rates, remission rates, and the median number of sessions/days required to reach response/remission were found to be comparable.
Efficacy has been further established in a prospective double-blind randomized controlled trial, in which 52 participants aged 60-85 with Major Depressive Disorder (MDD) received either active or sham high-dose Deep TMS for 20 sessions. The remission rate was significantly higher in the active group compared to sham (ITT: 40.0% vs. 14.8%, PP: 50.0% vs. 14.8%), with a Number Needed to Treat (NNT) of 4.0 (ITT) and 2.8 (PP). Response rates were also higher in the active group (ITT: 44.4% vs. 18.5%, PP: 55.0% vs. 18.5%), with NNTs of 3.9 (ITT) and 2.7 (PP). These findings are comparable to those of the pivotal MDD trial of middle-aged adults treated with Deep TMS.
Deep TMS has not been shown to cause any systemic side effects. A 2007 study in Clinical Neurophysiology confirmed this, finding Deep TMS to be a well-tolerated treatment with no systemic side effects.
Individuals undergoing Deep TMS treatment may experience a slight discomfort during the procedure, with some reporting a tapping sensation in the area being treated. In the double-blind randomized controlled trial of 52 late-life depression patients, no serious adverse events were observed. The only side effect significantly more common in the active Deep TMS group than sham was pain (16.0% vs 0%). In addition, 56% of patients receiving active Deep TMS treatment experienced headaches after treatment, though this was not significantly different from the sham treatment group (37%).
BrainsWay’s unique, patented H-Coil technology is held inside a cushioned helmet fitted onto the patient’s head. Upon activation, the H-coil produces magnetic pulses that regulate the brain’s neural activity.
BrainsWay’s Deep TMS sessions for depression last approximately 20 minutes. A Deep TMS treatment plan usually requires daily sessions over four weeks, followed by periodic maintenance sessions.
The following graphic details Deep TMS’s treatment protocol, with its Acute and Continuation phases:
Ronda’s Story
Hear how a retired special education teacher experiencing late-life depression finally overcame her symptoms after years of various antidepressants after BrainsWay Deep TMS depression treatment with Dr. Walter Duffy of Premier Psych (Alivation Health).
Check out additional testimonials of patients and healthcare providers in our video gallery.
Depression is a neuropsychiatric disorder that is expressed in emotional, physiological, and behavioral...
Deep TMS is the only TMS system FDA-cleared to reduce comorbid anxiety symptoms in adult patients with...
BrainsWay Introduces the First FDA Cleared (De-Novo), Non-invasive, Medical Device for the Treatment...