Journal: Biological Psychiatry (2022)
Authors: M Harel, I Perini, R Kämpe, U Alyagon, H Shalev, I Besser, R Kampe, WH Sommer, M Heilig, A Zangen
Background:
Alcohol addiction is associated with a high disease burden, and treatment options are limited.
Objective:
In a proof-of-concept study, the authors used Deep TMS to target circuitry associated with the pathophysiology of alcohol addiction and evaluated clinical outcomes and associated neural signatures using fMRI.
Methods:
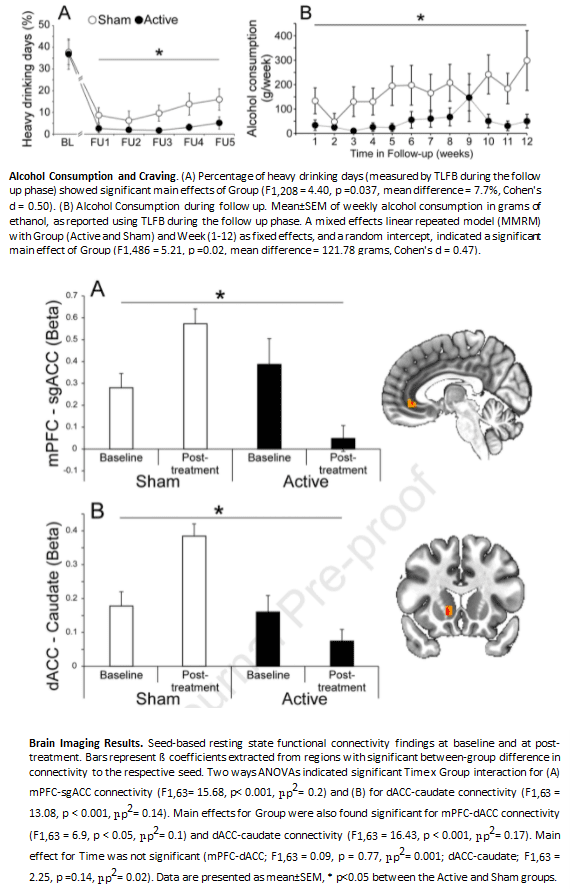
In this double-blind, sham-controlled, randomized clinical trial the authors evaluate clinical and neurobiological effects induced by high-frequency (10Hz) Deep TMS over 3 weeks of treatment and 12 weeks of follow-up. Clinical response is determined using self-report levels of craving and alcohol consumption validated by urine measures, while fMRI is employed to identify alterations in brain connectivity.
Results:
Both craving following treatment and pHDD during follow-up were significantly lower in the Active vs. Sham control group (pHDD=2.9±0.8% vs 10.6±1.9%, p=0.037). Active Deep TMS was associated with decreased resting state functional connectivity of the dorsal ACC with the caudate nucleus, and decreased connectivity of the mPFC to subgenual ACC.
Conclusions:
This study provides initial proof-of-concept for Deep TMS targeting midline frontocortical structures as a treatment for alcohol addiction. The data strongly supports a rationale for a full-scale confirmatory multicenter trial. Therapeutic benefits of Deep TMS appear to be associated with persistent changes in brain network activity.