Dealing with depression can significantly hinder one’s life in a number of ways. In addition to the symptoms characteristic of this mental health condition, such as negative and often overwhelming emotions, depression can harm one’s perception of self-worth, manifest in bouts of suicidal ideation, harm relationships with loved ones, negatively impact the ability to hold down a job, and accumulate large treatment costs. These reasons bring many individuals to consider cutting edge therapies, such as Deep TMS, as a treatment course that has the potential to offer them relief.
New information, studies, programs and treatment options for depression are more abundant than ever, making this diagnosis significantly more manageable. Individuals battling and dealing with depression are encouraged to learn and discover the different facets that are related to and might affect their condition. Additionally, it is highly advisable to consult your doctor to assess if you meet the requirements of a major depressive disorder diagnosis, and discuss the available treatment options that might be right for you.

Depression, or major depressive disorder (MDD) as it is defined by the American Psychiatric Association, is a mood disorder marked by a substantial decrease in quality of life, in a number of different areas.
Emotionally, depression is characterized by feelings of sadness, emptiness, loneliness and a lack of hope or pleasure. It is also marked by thoughts and actions that significantly hinder one’s daily level of functioning.
Furthermore, depression manifests in a myriad of emotional and behavioral symptoms that disrupt the individual’s daily functioning. These may include persistent feelings of worthlessness, guilt, or despair, amplifying the sense of emotional distress. Accompanying these emotions are often physical manifestations such as changes in appetite, sleep disturbances, and fatigue, further exacerbating the burden of the condition.
Moreover, depression can erode motivation and concentration, impairing cognitive abilities and impairing decision-making processes. Left unaddressed, these symptoms can perpetuate a vicious cycle, deepening the individual’s sense of despair and isolation. Thus, understanding the multifaceted nature of depression is crucial for tailoring effective therapeutic interventions and fostering holistic healing.
A number of treatment options have been proven to safely and effectively treat depression. These include Deep TMS, psychopharmacology (medication) and psychotherapy, which will be elaborated on later.
Read more about MDD treatment options.
Despite being often used interchangeably, depression and sadness are actually different from one another. Similarly, and though they share certain traits, a distinction should be made between depression and grief.
Sadness—an emotional pain characterized by a lacking or longing sensation—is a common part of the emotional spectrum and the human experience at large. Though sadness can affect an individual’s well-being, it normally does not significantly hinder their ability to function in day-to-day life for an extended period of time. Depression, however, can cause a much greater emotional disruption to an individual’s quality of life, and for much longer stretches of time.
Grief—an emotional destabilization process that happens during bereavement—centers around a feeling of emptiness due to the loss of a loved one, ability, object or even an idea. Like sadness, grief is not considered a disorder. While grief includes a preoccupation with what has been lost, depression turns its focus back to the individual experiencing it, thus causing a large amount of self-criticism. Additionally, though depression can stem from grief or appear with it, it is usually more severe than grief.

Both sadness and grief typically occur as reactions to a known event or experience, with the individual ultimately being able to move past them without either these adverse emotions becoming a constant fixture in their life. Depression, however, can emerge without being linked to a recognizable source, and may become a recurrent theme in life; as a result, an individual can experience depression without understanding what brought it on.
Depression affects about one in 15 adults (or 6.7%) of the adult population. In the US, 17.3 million adults (7.1%) have reportedly experienced one or more depressive episodes during their lifetime.
Disorder Symptoms: According to the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-V), major depressive disorder (MDD) is characterized by extended periods of sorrow, anhedonia (a lack of happiness), or an absence of hope that things might improve. Additional symptoms include erratic sleep patterns, significant weight change when not dieting, low self-confidence, suicidal ideation, excessive guilt and a lack of energy.
The different symptoms of MDD can cause significant impairment in several areas of life, such as self-worth, social and occupational spheres and personal hygiene.
It should also be noted that an MDD diagnosis should only be considered when the symptoms associated with it are not the result of a medical condition or substance abuse (for example, in cases where weight loss is the result of cancer treatment). Additionally, individuals who have experienced a manic or hypomanic episode would not typically receive an MDD diagnosis.
Symptom Severity and Episode Recurrence: The level of severity and single vs. recurring episodes are also taken into consideration when assessing MDD. The condition’s severity spectrum ranges from mild to severe, and also examines possible psychotic features that may arise.
Risk Factors: Several factors have been shown to increase the chances of developing MDD. They include a temperamental inclination, genetics, one’s childhood environment, life events and the existence of additional mental disorders or medical conditions.
Related Mental Health Conditions: Depression can emerge together with other psychiatric disorders. For example, many individuals battling obsessive-compulsive disorder (OCD) or post-traumatic stress disorder (PTSD) also cope with symptoms of depression.
Throughout human history, and long before our current definition for major depressive disorder, the concept of depression, seen as a mood disorder characterized by feelings of emptiness and sadness, had been repeatedly molded and reconceived. As society changed, so did its view of depression, with philosophers, social theorists, artists, and laypeople all adding their own input into what constitutes this hard to pin down experience, which, for many, is part of their daily lives.
Read more about the history of depression.
These days, major depressive disorder is seen as a mental condition whose development can be traced back to a number of factors. A much earlier perception of depression, though, emphatically found its roots in a physical condition.
Considered the “Father of Medicine,” Hippocrates (460 – 370 BCE) was an ancient Greek physician whose theoretical work saw all physical mechanisms (and eventually, personality types) as caused by internal bodily fluids that he called humors.
Melancholic Personality Type, according to the humors theory, was created by an excess of black bile. This personality type was similar to how we currently view the depressive state, with melancholics described as introverts, deep thinkers, and those who typically relate to the sadder side of the emotional spectrum.

It was 19th Century German psychiatrist Emil Kraepelin who first referred to melancholia as “depressive states,” due to the low mood that characterizes it. Unlike the humors theory, Kraepelin saw depression as caused by a devastating emotional or mental experience. He divided depression into two categories, based on its source: if it was brought on by an external tragedy, such as the death of a loved one, it was considered a form of “manic depression” and expected to pass; depression that did not stem from a known, external cause was understood to have “grown” out of the individual’s psyche, and as such considered a break from reality, similar to present-day schizophrenia.
Sigmund Freud, the father of psychoanalysis, wrote about depression in his 1917 essay, Mourning and Melancholia. In it, he defined melancholy as built around a sense of loss where the lost object itself is unknown, following the mental process of repression.
Freud stated that depression interferes with the normal mourning process, thereby causing the individual experiencing it to feel a general sense of sadness, believing the anguish and hopelessness they are feeling to be inescapable.
Opting for a more empirically-based approach to depression over Freud’s psychoanalytic theory was Swiss psychiatrist Adolf Meyer. Eventually rising to the position of President of the American Psychiatric Association, Meyer pushed the mental health community into considering biological factors, as well as mental and familial ones, as potential sources of depression.
Around the mid-20th Century, the medical and mental health communities began a concerted effort to reach a consensus on how to identify and treat mental health conditions, based on data from the field. As a result, two main systems emerged: the International Statistical Classification of Diseases, Injuries and Causes of Death (ICD) in 1949, and the Diagnostic and Statistical Manual of Mental Disorders (DSM) in 1952. The ICD examines physical and mental ailments and is used across the globe, while the DSM focuses on mental disorders and is mainly used in the US. Both publish updated editions that reflect research discoveries and changes in society.
The mid-20th Century also saw a revolution in major depressive disorder healthcare, when antidepressant medications were introduced as a viable treatment method. The proven efficacy of antidepressants underscored the biological and genetic factors related to this condition, while being able to offer many patients significant symptom relief.
Read more about the benefits and possible side effects antidepressant medication can cause.
Cognitive psychology grew out of the “cognitive revolution” of the 1950s-’80s, which aimed to understand the mind and its mental processes through empirical tools. A leading figure in this movement was psychiatrist Aaron Beck, whose BDI assessment tool for depression, as well as Beck’s cognitive triad for depression are still used today.
Looking at the different factors contributing to depression, Beck posited that one’s beliefs about themselves, the world and the future influenced one another and decided their level of susceptibility to depression: as such, an individual believing they are the ones to blame for their depression, that the world is a fundamentally lonely place, and that none of this will change, are likely to develop depression.
Though most research has focused on the adult population, depression can also occur during other stages of life. As such, special care should be given to those in additional age groups, such as children, adolescents and senior citizens, whose depression can manifest through symptom patterns of their own.
Depression Among Children: With their communication skills, introspective abilities and view of the world still in development, children often find it harder to clearly express what they are going through. As a result, they may struggle to convey their emotional world to parental or adult figures.
Rates of depression among children have been steadily rising in the last several years, with up to 3% of US children said to develop depression. Children with depression may show signs of irritability, clinginess, complain of physical aches and pains, display emotional outbursts, run away from home, be prone to accidents, refuse to go to school or underperform academically, or go through significant weight changes.
Depression Among Teenagers: Adolescence is a time when individuals transition out of the more dependent and unaware state of childhood, and begin exploring the different roles they may come to identify with later in life. This period of exploration can bring with it new passions and excitement, but it can also cause confusion, feelings of self-doubt, and for many, their first experience with depression.

Up to 8% of US adolescents are thought to develop depression. Teenage depression may manifest itself through believing they are misunderstood, an increased irritability, poor attendance and underperformance at school, significant weight change, self-harm and risk-prone behavior, or experimenting with illegal and harmful substances.
Depression Among the Elderly: With child rearing and career development for the most part behind them, and loneliness at times becoming a more central part of their lives, many senior citizens develop depression. Though less common than in younger adulthood, depression among the elderly carries its own risks and symptoms, which if left unaddressed could become fatal. Additionally, the appearance (or even suspicion) of Alzheimer’s or dementia could cause a depressive condition to be overlooked, with its symptoms ascribed instead to the above-mentioned conditions.

Depression in older adults appears in 1%-5% of this population, but rises to 11.5% if they are hospitalized, and to 13.5% if they require home healthcare, in part due to their perceived loss of independence. Symptoms of elderly depression include impaired memory, personality changes, a loss of appetite, fatigue, and physical aches and pains. Suicide attempts are also symptomatic of elderly depression, and are more commonly linked to depression than among younger adults.
Major depressive disorder can be treated through a number of approaches that can broadly be grouped into three categories: medical devices, medication, and psychotherapy.
A number of cutting edge medical technologies have been shown to effectively treat depression. Out of the different options available today, ECT, TMS and Deep TMS have gained a greater level of professional and public recognition.
ECT: Electroconvulsive therapy is a medical treatment that induces a brief set of seizures to stimulate the brain and affect its neural functioning. The treatment was originally used for schizophrenia, before researchers during the 1960s-‘80s found it to be even more effective in treating mood disorders, and in particular depression. As a result, today it is primarily used to treat this condition.
The treatment’s effectiveness in treating depression has been well-established, especially in cases of severe depression. That said, it does hold several disadvantages: first, ECT necessitates full sedation under anesthesia, which complicates its recovery process; second, the procedure can cause short-term memory loss, which deters many potential patients; finally, ECT has gained a rather negative public perception, much of it due to misinformation that characterizes it as a traumatic, personality-altering procedure.
TMS: Transcranial Magnetic Stimulation has been publicly available since 2008, as a non-invasive option for patients with major depressive disorder. The procedure sends out a series of electromagnetic pulses from a figure-8-shaped handheld device. The pulses are then used to regulate the neural activity of brain structures shown to be related to depression.
Though TMS has been proven to be safe and effective in alleviating symptoms of depression, this original, standard form of TMS has been shown to hold certain limitations: first, the 8-coil’s relatively narrow scope means that only a few brain structures can be reached with each individual pulse. For this reason, standard TMS sometimes suffers from targeting issues, and may miss some of the relevant structures; additionally, standard TMS has trouble directly stimulating deeper structures in the brain structures, which can also potentially decrease its efficacy.
Deep TMS: Deep Transcranial Magnetic Stimulation, or Deep TMS, is an advancement of the standard, figure-8 TMS treatment that answers some of the issues raised with its predecessor. First introduced in 1985, Deep TMS is similarly a non-invasive treatment that utilizes a magnetic field to safely regulate the neural activity of brain structures shown to be associated with depression, as well as other mental health conditions. Deep TMS does not require anesthesia and can be incorporated into one’s daily routine.
Deep TMS addresses standard TMS’s scope limitations through its own, patented H-Coil technology, which is held inside a cushioned helmet fitted onto the patient’s head. The magnetic fields produced by the H-Coil not only manage to reach wider areas of the brain, but also directly stimulate structures located in deeper regions of the brain, which contributes to the treatment’s efficacy and has repeatedly been shown to safely alleviate symptoms of depression. It is this combination of effectiveness and its adherence to high safety standards that granted Deep TMS its FDA clearance status in 2013 for treating depression. It is also the only non-invasive medical device to be given FDA clearance status for treating OCD.
Watch more deep TMS depression patient testimonials
Deep TMS has not only been proven to effectively alleviate MDD symptoms, but can also be combined with any type of medication, thanks to its non-invasive treatment process. A 2019 study published in the Journal of Psychiatric Research underscored this, finding that the treatment achieved significantly higher remission rates when combined with pharmacotherapy, as opposed to pharmacotherapy alone.

As a non-invasive treatment option, Deep TMS provides a safe form of therapy for a number of mental health conditions, without the need for anesthesia. During the Deep TMS process, a cushioned helmet holding its patented H-Coil technology is fitted onto the patient’s head. An electromagnetic field is then activated through the H-Coil, sending out magnetic pulses able to directly and safely stimulate neurons in deeper brain structures found to be associated with the targeted condition.
Deep TMS has also consistently been found to be a safe treatment without any substantial, lasting or systemic side effects. As one example, a 2007 study published by Clinical Neurophysiology concluded that Deep TMS is well-tolerated and does not cause any adverse physical or neurological side effects.
In addition to being able to reach deeper brain structures directly, Deep TMS manages to cover a wider area of the brain. This grants Deep TMS the ability to concurrently regulate more brain structures associated with the relevant mental health condition.

Deep TMS’s direct activation of deeper brain structures, in addition to its wider scope, ensure a high level of efficacy without the need to increase pulse intensity to a level that might risks undesirable side effects. It also helps ensure the targeted brain regions are captured without necessitating secondary navigation equipment.
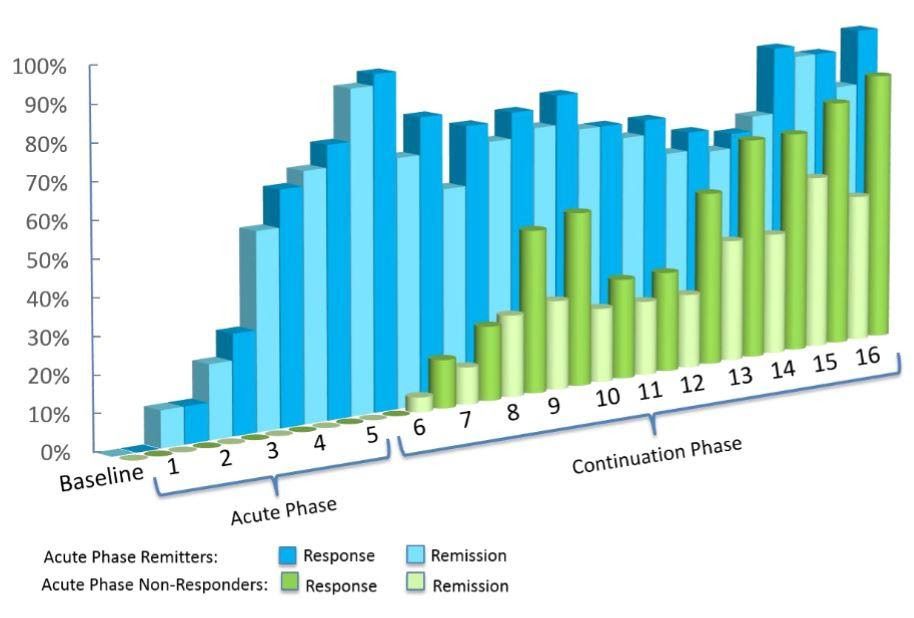
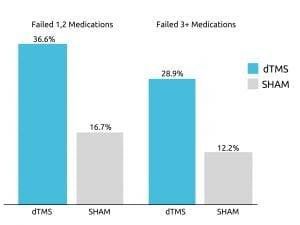 Deep TMS’s efficacy was highlighted in a 2015 multicenter, sham-controlled study published in World Psychiatry. The study found that roughly one out of three patients with treatment-resistant MDD achieved remission after four weeks of Deep TMS treatment during the acute phase.
Deep TMS’s efficacy was highlighted in a 2015 multicenter, sham-controlled study published in World Psychiatry. The study found that roughly one out of three patients with treatment-resistant MDD achieved remission after four weeks of Deep TMS treatment during the acute phase.
The study additionally found that close to 80% of patients who did not immediately respond during the acute treatment phase, went on to experience an improvement during the following continuation phase.
Deep TMS was found to have an even higher efficacy level among individuals receiving treatment in a real-life setting, outside a rigorous clinical study. From the recorded data of over 1000 participants undergoing major depressive disorder treatment, around 75% achieved a clinical response due to Deep TMS treatment, with one out of two patients achieving remission.
Due to its healthcare benefits, Deep TMS has been granted FDA clearance status for both MDD and OCD. It is also CE-marked in Europe, to treat these and a number of other mental health conditions.
Additional device treatment options for depression are still being explored, to varying clinical results. Examples include vagus nerve stimulation (VNS), transcranial direct current stimulation (TDCS), magnetic seizure therapy (MST) and deep brain stimulation (DBS).
Antidepressant medication has been found to be an effective form of major depressive disorder treatment, though it may cause adverse side effects and requires an adjustment period before assessing its efficacy. Possible medication side effects include weight gain, nausea and sexual dysfunction, blurred vision and increased heart rate.

Antidepressants work by affecting the brain’s secretion of neurotransmitters, which are chemicals that transport information between nerve cells. Over time, several different generations of antidepressants have been approved for the public, with each targeting depression symptoms through different neural pathways and methods of affecting them.
At present, the three most commonly prescribed antidepressants are tricyclics, SSRIs and SNRIs. All three classes of medication have been shown to effectively alleviate symptoms of depression, though their side effects could prove to be severe, and must be taken for several months before their efficacy and overall effect can be gauged.
Ketamine is mainly given by infusion or as a nasal spray. Possible side effects include high blood pressure, nausea, vomiting, perceptual disturbances and (rarely) dissociation. Only the ketamine nasal spray has been FDA-approved to treat depression. Similar to opioids, ketamine does have addictive properties. As a result, individuals with a history of alcohol or drug abuse should seriously take this into account while weighing this treatment option with their doctor.
As with all forms of major depressive disorder treatment, it is essential that anyone considering a new therapy consult with a licensed professional who can further illuminate the different options and any possible effects they might have. Specifically with medication, questions of dosage, adjustment periods, alertness to potential side effects and reactions to combining different types of therapy should be raised and discussed with a trained and experienced expert.
Psychotherapy operates as a collaborative process, rooted in empathetic dialogue between the patient and a trained mental health practitioner. These conversations delve into the intricate layers of the patient’s psyche, aiming to uncover the nuanced intricacies of their lived experiences. They explore not only the patient’s worldview and beliefs but also the dynamics of their interpersonal relationships, tracing the contours of significant connections and pivotal life events. Additionally, psychotherapy delves into the intricate workings of the patient’s mind, dissecting thought patterns, emotional responses, and coping mechanisms. It seeks to unearth the underlying triggers and challenges that shape the patient’s mental landscape, fostering insight, healing, and growth.

Psychotherapy has been shown to offer relief from symptoms of depression. That said, the diverse array of psychotherapeutic theories and techniques can make choosing a treatment course quite challenging. Those who wish to begin psychotherapy are advised to look for a mental health professional they feel relatively comfortable, and could possibly develop a personal connection with. Additional aspects to consider are the therapist’s location, their availability, and the treatment’s cost.
Out of the many different forms of psychotherapy available to patients with depression, one branch has been recognized for its clinically proven ability to offer significant depression symptom relief: psychodynamics. FDA-approved for treating depression due to its safety and efficacy, psychodynamic therapy examines how the patients’ past and present, the central relationships in their lives, the use of defense mechanisms and other aspects of their internal world connect with one another.
When treating depression, psychodynamic therapy looks to better understand what factors in the patient’s life contributed to the appearance of this condition. Through progress within this form of therapy can at times be slow and gradual, the insight that can be gained through this journey lends itself to more essential change, as root causes are uncovered, examined and in many cases, forgiven, so as to allow the patient to move on from them.
Psychodynamics is in itself a diverse branch within psychotherapy. It is comprised of the work of many different theorists, as well as several theoretical schools and movements. While some of its thinkers and practitioners have attempted to meet their patients’ emotional needs within a therapeutic setting, others have focused on helping their patients develop a better understanding of themselves, allowing the patient to decide how they wish to best fulfill their needs. Whatever their style, focus or main sources of inspiration are, psychotherapists wish to offer their patients a more beneficial experience in the world, through communication, comprehension and basic compassion.
Among depression’s various symptoms, loneliness and the belief that the emotional pain induced by this condition cannot be understood by others can cause those battling depression to isolate themselves, spending increasingly more time alone.

In an effort to battle the loneliness experienced by individuals with depression, support groups have been made more available. Offered by mental health centers, religious groups, and support networks founded by individuals with depression, support groups for depression provide an at times essential source of camaraderie to those facing this condition. By creating a more empathetic environment, these groups can help its members feel less isolated, more understood, and part of a community that can pull them through some of their darkest hours.
Organizations such as the Anxiety and Depression Association of America (ADAA), the Depression and Bipolar Support Alliance (DBSA) and Mental Health America (MHA) all offer group support, as well as refer individuals to local mental health professionals.
Additionally, with the development and increased prevalence of online communities, healthcare websites and social media platforms now host a variety of groups geared toward connecting between those battling depression. Facebook group Defeat Depression, personal Instagram accounts that detail the struggles that go into facing this condition, or social media hashtags like #MentalHealthMatters manage to reach many online users, begin conversations among those looking for someone to talk to and bring information, awareness and support to those who can benefit from them.