Journal: Current Behavioral Neuroscience Reports
Authors: Nan Zhang, Yu Mo, Xian-Jun Lan, Qi-Man Liu, Wen-Xiu Li, Xing-Bing Huang, Hua-Wang Wu, Shi-Chao Xu, Shu-Yun Li, Xin-Hu Yang, Wei Zheng
Background:
This systematic review aimed to evaluate and compare the safety and effectiveness of deep transcranial magnetic stimulation (dTMS) with high-frequency repetitive transcranial magnetic stimulation (HF-rTMS) for individuals diagnosed with major depressive disorder (MDD). The study was motivated by the inconsistent findings of prior studies comparing dTMS and HF-rTMS for depression treatment. The researchers hypothesized that dTMS would yield a significantly higher response rate than HF-rTMS in adult patients with MDD.
Objective:
The objective of this systematic review was to evaluate and compare the safety and effectiveness of dTMS with that of high-frequency rTMS (HF-rTMS; ≥10 Hz) in individuals diagnosed with major depressive disorder (MDD).
Methods:
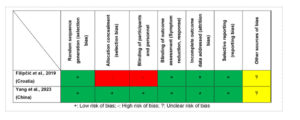
The review searched Chinese and English databases for RCTs comparing dTMS and HF-rTMS. The overall antidepressant response and remission rates were the co-primary outcomes. The systematic review included two RCTs that compared the efficacy and safety of dTMS versus HF-rTMS for treating MDD in adults.
Results:
Two RCTs met the inclusion criteria, with a Jadad score of ≥ 3, indicating high quality. The overall antidepressant response rate was significantly higher in the dTMS group (60.0%) than in the HF-rTMS group (41.7%). The results of this systematic review showed that dTMS provides a more pronounced overall antidepressant response than HF-rTMS, but causes more muscle twitching/spasms or jaw pain incidences. Both RCTs had similar rates of other adverse events and discontinuation.
Conclusions:
dTMS leads to a better antidepressant response than HF-rTMS, although both interventions have favorable safety profiles. However, more RCTs using rigorous methodologies are warranted. The conclusions of this systematic review are that dTMS is associated with a better antidepressant response than HF-rTMS in adult patients with MDD, although both treatment modalities have favorable safety profiles.